Hemolytic Anemia
Symptoms/Signs of Hemolytic Anemia
- Fatigue, weakness, dyspnea
- Dark, coca-cola coloured urine (hemoglobin --> methemoglobin over time); red urine (rapid)
- Flank pain
Laboratory Features
- Normocytic/macrocytic hyperproliferative anemia
- Evidence of RBC destruction:
- increased urobilinogen in urine and stool, increased serum AST, increased serum unconj bilirubin, increased serum LDH and decreased serum haptoglobin
- Increased serum free hemoglobin, hemoglobinuria (intravascular or severe extravascular)
- bilirubin can be normal in predominantly intravascular hemolysis (formed by the RES)
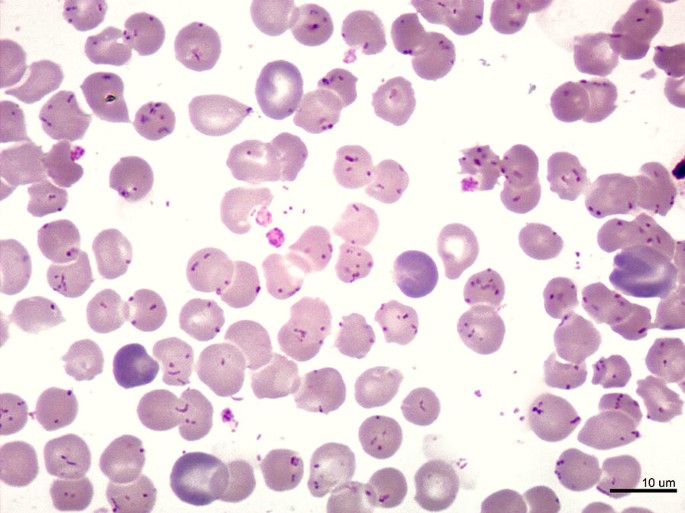
- Smear: reticulocytosis, polychromasia, nucleated RBCs. Watch out for schistocytes, spherocytes, bite cells.
Clinical Sequelae
- Folate deficiency
- Cholelithiasis with pigmented gallstones
- Splenomegaly
- Leg ulcers
- Pulmonary hypertension
Approach to Hemolytic Anemia
Hemolysis can be intravascular, extravascular (spleen), or both. When the RBC damage is severe enough to cause immediate lysis in the intravascular space, this releases free hemoglobin into the bloodstream. When the damage is not that severe, the RES removes the affected cells, which generates unconjugated bilirubin from hemoglobin breakdown.
Disorders of ineffective hematopoiesis can lead to premature intramedullary lysis of erythroid progenitors, which can mimic hemolytic anemia.
The following approach is also is based on WHY the hemolysis occurs:
- Intrinsic RBC issues
- Membrane defects
- Enzyme defects (G6PD deficiency, PK deficiency)
- Hemoglobinopathies (Sickle cell anemia, Thalassemia, Hemoglobin C disease, unstable hemoglobin)
- Immune-mediated
- Autoimmune (warm/cold)
- Alloimmune (hemolytic transfusion reactions)
- Complement-mediated
- Hypersplenism
- Mechanical issues
- TMA
- Mechanical heart valves
- Other
- Malaria, babesiosis, other tick-borne diseases
- Wilson's Disease
Intrinsic RBC Defects
Hemoglobinopathies
- Sickle cell disease
- Thalassemia - anemia with microcytosis and hypochromia, possible target cells and teardrop-shaped cells, basophilic stippling, and nucleated RBCs
- Hemoglobin C disease - homozygous is generally benign with mild hemolytic anemia, target cells, spherocytes, and splenomegaly. In combination with sickle cell disease, much more severe manifestations
- Unstable hemoglobins - SNPs that reduce hemoglobin stability. Formation of Heinz inclusion bodies that lead to intravascular and extravascular hemolysis
Enzyme Deficiencies
- G6PD deficiency - XLR mutation that leads to anisocytosios, polychromasia, Heinz bodies, and characteristic poikilocytes/"hemighost" cells.
- Pyruvate kinase deficiency - deficiency in the enzyme in the final step of glycolysis. Variable presentations, mostly leads to extravascular hemolysis. Peripheral smears are nonspecific. Splenectomy can be beneficial.
Membrane Defects
- Hereditary spherocytosis - wide spectrum of disease, can be very mild to very severe. Leads to increased MCHC. On smear, there are spherocytes. Osmotic fragility testing can be done. Molecular testing is the definitive diagnostic test.
- Hereditary elliptocytosis (ovalocytosis) - protects against malaria. Clinically similar to hereditary spherocytosis. On smear, there are elliptocytes which are oval/elliptical in shape.
- Hereditary stomatocytosis & hereditary xerocytosis - these are conditions of abnormal RBC hydration. Autosomal dominant.
- Stomatocytosis: overhydration. -MCHC, +osmotic fragility
- Xerocytosis: dehydration. +MCHC, -osmotic fragility
- Avoid splenectomy in both of these conditions as it increases the risk of thromboembolism
Immune-Mediated
Autoimmune Hemolytic Anemia (AIHA)
See [[Anemia/Autoimmune Hemolytic Anemias]].
Alloimmune Hemolytic Anemia
These are typically DAT positive but from non-autoimmune causes. Alloantibodies can develop after exposure to pregnancy or exposure to blood products. These are typically IgG and result in delayed-onset mild extravascular hemolytic anemia.
- Delayed hemolytic transfusion reaction
- Hemolytic disease of the newborn
- Drug-induced hemolytic anemia
- Alloimmune hemolysis post solid organ or allogeneic SCT
DAT can also be positive in the context of other causes (SLE, renal diseases, IVIg, ATG)
Drug-Induced
- AIHA (methyldopa)
- TMA (quinine)
- oxidative hemolysis (dapsone in G6PD)
- antibiotics (beta-lactams)
Hypersplenism
Splenomegaly can lead to hemolytic anemia by virtue of sequestration and RBC destruction. Typically is a mild anemia and associated with other cytopenias.
Spur Cell Anemia
This is an extravascular hemolytic anemia due to chronic liver disease and alterations in the cholesterol ration in the RBC membrane. Leads to moderate-severe anemia.
Paroxysmal Nocturnal Hemoglobinuria
Rare but life-threatening disease , most common in the 4th decade of life. Deficiency of CD55 and CD59 membrane proteins leads to complement-mediated destruction, intravascular hemolysis.
Morning hemoglobinuria + venous thrombosis + pancytopenia.
Toxic Hemolytic Anemia
Dapsone, lead poisoning (abdominal pain, peripheral edema, basophilic stippling), snake/spider/bee/wasp stings and bites, Wilson's disease, and arsenic poisoning (arsine gas inhalation, arsenic ingestion).
Traumatic Hemolytic Anemia
- TMA
- TTP
- HUS
- DI-TMA
- Malignant hypertension
- HELLP syndrome
- Severe B12 deficiency
- Intravascular hardware (valves)
- March hemoglobinuria
Infectious Hemolytic Anemia
- Malaria
- EHEC/HUS
- Clostridium perfringens
- Mycoplasma pneumoniae
- HiB
- Babesiosis
- Bartonella bacilliformis (Carrion's disease, Oroya fever)
- transmitted through bites of certain phlebotomine sand flies in the Andean valleys of Peru and in some areas of Ecuador and southern Colombia
- these bacteria directly invade RBCS leading to intravascular and extravascular hemolysis with severe and acute anemia
- smear can show intraerythrocytic bacilli:
- Patients then develop Verruga peruana (angiogenic lesions):

References
- IM Review Slides
- Frameworks for Internal Medicine